How Your Body Uses Glucose: 4 Tips for Optimization and Regulation
The pancreas, which is part of both the digestive system and the endocrine system, is the organ most directly involved in regulating our blood sugar levels.1 In healthy people with blood glucose levels in a normal range, it’s responsible for producing enzymes to help break down food as well as producing the hormone insulin, which helps to control blood sugar levels more directly. Let’s follow the path of dietary sugars – from ingestion to utilization – to better understand how our bodies take in and use those sugars every day.
Blood Glucose Absorption and Metabolism
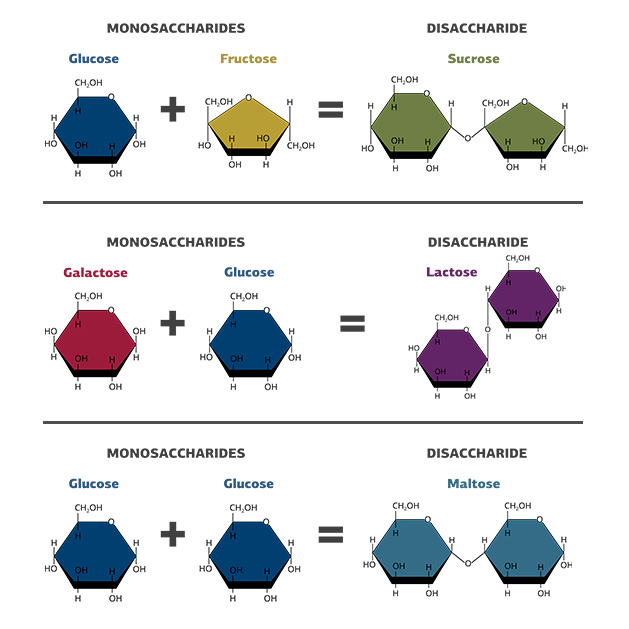
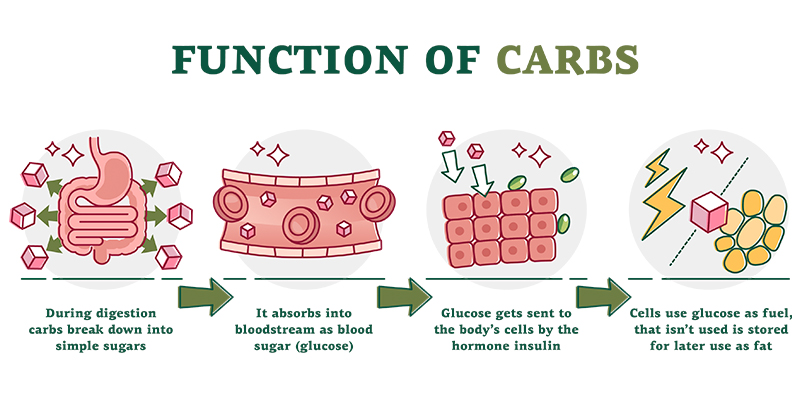
Food provides fuel to our body. Carbohydrates – sugars, specifically – provide quick, easily converted forms of fuel for the body, beginning in the digestive system. This is compared to proteins and fats, which involve more complex processes to break down. Carbohydrate digestion begins in the mouth with enzymes in our saliva that begin to break down large pieces of food into smaller components. This process continues into the stomach and intestines where the food is broken down into such small molecules of sugars that they can be absorbed into the blood stream. These molecules of sugar (fructose, galactose, and glucose) are called monosaccharides, and are the smallest unit of sugar. In various combinations, they compose more common sugars that you might know:
Galactose + Glucose = Lactose (found in milk)
Glucose + Glucose = Maltose
Monosaccharides then travel to the liver where they can be processed and distributed throughout the body as needed. Working as the command center for the body, the liver translates all the inputs from the body to assess what it needs and sends glucose out as needed for functions like exercise or studying or even sleeping. When blood sugar reaches its destination, proteins called glucose transporters will travel to the surface of the cell to create a “tunnel” for glucose to go through. This final step is how sugar “leaves” the blood and can carry out important functions in the many organs of the body.
Blood Glucose Regulation
Because blood sugar keeps us alive and functioning, the body aims to closely monitor and maintain blood sugar levels. Blood glucose is regulated primarily through two hormones - insulin and glucagon – produced in the pancreas as part of the endocrine system.
Regulation with Insulin
Let’s start with insulin. We may think of insulin as “bad” because we hear terms like insulin resistance as part of metabolic challenges. But insulin is simply a signal to the body that it can grow because there are sufficient nutrients (sugar in this case) present. This can obviously become an issue when there is an overabundance of nutrients, but your body needs insulin to grow and function.
Let’s zoom in on how this regulation happens in bodies of those who have normal blood glucose levels. Upon absorption, glucose travels in the blood, and some will arrive at the pancreas. The pancreas detects glucose and releases insulin from beta cells in response.2 Insulin then travels throughout the body where it results in a blood glucose-lowering effect. It lowers blood glucose by helping cells in the body import glucose, therefore removing it from the blood and into organs that need it for fuel.2 Specifically, when insulin reaches the outside of a cell, it initiates a signaling cascade that results in glucose transporters coming to the cell surface where they provide an avenue for glucose to enter.2 Think of it as a lock and key - insulin is the key that unlocks the cell so
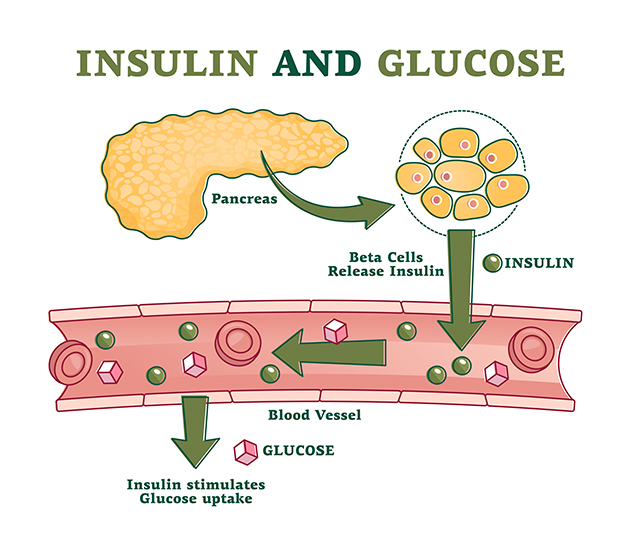
To summarize, after a meal, your healthy body will absorb sugar which signals to the pancreas to release insulin. Insulin then travels throughout the body and tells cells to import glucose, removing it from the blood.
Regulation with Glucagon
But what happens if you’ve skipped breakfast or had an intense, long workout with little food beforehand? At this point, your body would probably be running low on blood sugar. This is where glucagon comes into play. Glucagon is also a hormone produced by the pancreas, but in the alpha cells instead of beta cells.2 Glucagon opposes the actions of insulin - it works to increase blood glucose levels.2 To prevent mixed messages, glucose stimulates insulin but inhibits glucagon. When blood glucose levels are too low, glucagon signals to the liver to convert stored glucose, called glycogen, into a usable form of glucose that can then enter the bloodstream and travel to cells that need it.2 Glucagon can also stimulate the liver to utilize amino acids or lipids in the body for conversion to glucose if needed. Glucagon is released in response to hypoglycemia, prolonged fasting, exercise, and high protein meals.3
Other factors affect the action of these hormones as well as other organs in the body to regulate blood sugar levels. Sleep, exercise, stress, meal composition and timing, and hormones can all affect how blood glucose is metabolized and regulated in the body. Read more in our post, 3 Unexpected Triggers for Your Body’s Blood Sugar to Rise
Glands in the Endocrine System That Influence Blood Glucose
The pancreas is the most important gland for controlling blood sugar levels because it produces both insulin and glucagon. However, there are other important glands that also help to regulate blood sugar levels. The adrenal gland can increase blood glucose levels when necessary, including emergency situations that activate the body’s fight-or-flight response.4 The thyroid gland is critical in regulating whole-body metabolism, including blood sugar levels.5 Although it does not secrete insulin or glucagon, issues with the thyroid gland can have a huge impact on blood glucose regulation.5 Finally, the pineal gland helps regulate sleep patterns via melatonin which can influence glucose regulation.6,7
Glucose Utilization
Glucose is the most efficient form of fuel for cells - meaning they can generate the most cellular energy currency per glucose molecule compared to fats or proteins. Cells in different organs will use energy from glucose for their own specific needs:
- The liver is one of the most important organs in the body when it comes to handling and processing blood sugar. It directly receives glucose that has been absorbed and directs it to be stored as glycogen, converted for glycosylation reactions (important for activity of proteins in the body), used as energy for the liver, or directed to other parts of the body that need it.8
- The brain accounts for about two percent of body weight but consumes nearly 20 percent of the energy the body makes from glucose.9 It uses glucose for diverse functions including learning, memory, synthesis of neurotransmitters, and maintenance of both neuronal and non-neuronal cells.9,10
- The kidneys produce glucose from other substrates (a process called gluconeogenesis), use glucose for energy needs such as filtering waste out of the blood, and reabsorb glucose that the body may need.11,12
- The lungs require glucose-derived energy for tasks including clearing the airways, constricting airways and blood vessels, and producing pulmonary surfactant, an important compound for lung health.13
- Retinal neurons in the eye support vision through a constant supply of glucose, especially in the dark.10
- Resting muscles are able to store glucose as glycogen but, during exercise, they are major consumers, breaking down glucose for energy for muscle contraction.14
- The intestines are critical to blood sugar maintenance as the primary site of absorption for dietary sugars, but they also use sugar. Glucose is used by intestinal cells to regenerate and differentiate, supporting the rapid turnover of intestinal cells.15
Glucose is critical for producing energy, which enables nearly every function throughout the body. But glucose is also an important cellular signaling molecule - meaning it works at the cellular level to initiate or transmit signals within or between cells. Glucose transporters are proteins that help exchange metabolites or signaling molecules in and out of cells. In order for many glucose transporters to work, glucose must be present. Therefore, glucose is also utilized at the cellular protein level to transmit signals and influence cellular health.16
Tips to Optimize the Way Your Body Utilizes Glucose
It can be overwhelming to focus on all the different body parts and systems that have a role in regulating blood sugar levels^ in already healthy bodies. Taking a broader view of metabolism and glucose utilization can point to several practical tips to help you optimize the way your body utilizes glucose:
- Choose complex carbohydrates when you can. Digestion of complex carbohydrates takes longer and results in a less intense rise in blood sugar levels.
- Consume carbohydrates with proteins and fats to minimize blood sugar spikes.
- Take a walk after a big meal. This will help your body shuttle glucose into cells and out of the blood.
- Pay attention to cues from your body that your blood sugar levels are too low or too high in order to keep them in a healthy range.
Now that we’ve discussed how the body utilizes glucose and tips to help that process, how do we know if our strategies are supporting wellness? Tracking blood sugar over time can help you figure out what affects your blood sugar levels and your body’s regulation of them. So what options are available?
A fasting blood glucose test provides important information on blood glucose levels without interference from a recent meal. If you want to be able to check your levels at home, you can use glucose strips and a glucometer for a real-time reading of your current blood glucose level. This allows for monitoring over time and different conditions to provide a clear picture of your body’s specific response. You may find that a healthy diet and lifestyle (possibly including supplements) helps keep your blood sugar levels stable and in a healthy range. Be sure to talk with your healthcare practitioner to better understand your body’s specific blood glucose pathways, your individual diet and lifestyle, and find out if adding a supplement that helps support healthy blood sugar levels^* could benefit you.
References
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/pancreas
- Röder, P.V., Wu, B., Liu, Y., Han, W. (2016). 48(3):e219.
- Rix I, Nexøe-Larsen C, Bergmann NC, et al. Glucagon Physiology. [Updated 2019 Jul 16]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279127/.
- Verberne, A.J.M., Korim, W.S., Sabetghadam, A., Llewellyn-Smith, I.J. (2016). Br J Pharmacol, 173(9):1425.
- Eom, Y.S., Wilson, J.R., Bernet, V.J. (2022). Diabetes Metab J, 46(2):239.
- Peschke, E., Bähr, I., Mühlbauer, E. (2013). Int J Mol Sci, 14(4):6981.
- Lima, F.B., et al. (1998). Am J Physiol, 275(6):E934.
- Adeva-Andany, M.M., Pérez-Felpete, N., Fernández-Fernández, C., Donapetry-García, C., Pazos-García, C. (2016). Biosci Rep, 36(6):e00416.
- Mergenthaler, P., et al. (2014). Trends Neurosci, 36(10):587.
- Wong-Riley, M. (2010). Eye Brain, 2:99.
- Girard, J. (2017). Nephrol Ther, 13 Suppl 1:S35.
- Gerich, J.E. (2010). Diabet Med, 27(2):136.
- Liu, G., Summer, R. (2019). Annu Rev Physiol, 81:403.
- Richter, E.A., Derave, W., Wojtaszewski, J.F.P. (2001). J Physiol, 535:313.
- Chen, C., et al. (2018). Front Biosci, 23(9):1721.
- Koepsell, H., Vallon, V. (2020). Pflügers Arch, 472(9):1107.
^already in a normal range









